Software program design plays a pivotal role in revolutionizing healthcare outcomes by streamlining processes, enhancing patient care, and improving overall efficiency, and CAR-REMOTE-REPAIR.EDU.VN is at the forefront of understanding this evolution. Embracing modern software solutions is crucial for healthcare professionals to stay competitive and deliver optimal patient care in today’s rapidly changing landscape. Explore advanced technology, enhance patient experience, and reduce human error with smart health programs!
Contents
- 1. What is Software Program Design in Healthcare?
- 1.1. Key Aspects of Software Program Design
- 1.2. Types of Healthcare Software
- 2. Why is Effective Software Program Design Important in Healthcare?
- 2.1. Enhancing Patient Care
- 2.2. Streamlining Workflows
- 2.3. Ensuring Data Security
- 2.4. Promoting Innovation
- 3. How Does Software Program Design Improve Patient Outcomes?
- 3.1. Diagnostic Accuracy
- 3.2. Treatment Effectiveness
- 3.3. Patient Engagement
- 3.4. Access to Care
- 4. What are the Key Components of Healthcare Software Program Design?
- 4.1. User Interface (UI) Design
- 4.2. Data Management
- 4.3. Security Protocols
- 4.4. Interoperability Standards
- 4.5. Compliance Regulations
- 5. How Do You Ensure Data Security in Healthcare Software Design?
- 5.1. Robust Security Protocols
- 5.2. Compliance Regulations
- 5.3. Regular Security Audits
- 5.4. Ongoing Security Training
- 6. What Role Does Interoperability Play in Healthcare Software Program Design?
- 6.1. Seamless Data Exchange
- 6.2. Improved Care Coordination
- 6.3. Enhanced Efficiency
- 7. How Can AI and Machine Learning Enhance Healthcare Software Program Design?
- 7.1. Diagnostic Accuracy
- 7.2. Personalized Treatment Plans
- 7.3. Automation of Administrative Tasks
- 7.4. Enhanced Research Capabilities
- 8. What are the Challenges in Healthcare Software Program Design?
- 8.1. Data Security and Privacy
- 8.2. Interoperability
- 8.3. Regulatory Compliance
- 8.4. Usability Issues
- 9. How Do Mobile Health (mHealth) Apps Fit Into Healthcare Software Program Design?
- 9.1. Remote Patient Monitoring
- 9.2. Medication Management
- 9.3. Telehealth Services
- 9.4. Health and Wellness Tracking
- 10. What Future Trends Will Shape Healthcare Software Program Design?
- 10.1. Increased Use of AI and Machine Learning
- 10.2. Adoption of Blockchain Technology
- 10.3. Expansion of Telehealth Services
- 10.4. Greater Focus on Personalized Medicine
- FAQ: Software Program Design on Health Care
- 1. What is the primary goal of software program design in healthcare?
- 2. How does effective software program design contribute to better patient outcomes?
- 3. What are the key components of healthcare software program design?
- 4. How do you ensure data security in healthcare software design?
- 5. Why is interoperability important in healthcare software program design?
- 6. What role do AI and machine learning play in healthcare software program design?
- 7. What are the main challenges in healthcare software program design?
- 8. How do mobile health (mHealth) apps fit into healthcare software program design?
- 9. What are some future trends that will shape healthcare software program design?
- 10. How can CAR-REMOTE-REPAIR.EDU.VN help me enhance my skills in healthcare software program design?
1. What is Software Program Design in Healthcare?
Software program design in healthcare involves creating and implementing software solutions that address specific needs within the healthcare industry, directly impacting patient care and operational efficiency. Software program design in healthcare involves the creation of tailored applications and systems that cater to the diverse requirements of medical professionals and patients, including electronic health records (EHRs), telemedicine platforms, and medical diagnostic tools. According to a 2024 report by the Healthcare Information and Management Systems Society (HIMSS), effective software program design not only enhances patient care but also streamlines administrative processes, reduces costs, and improves data security, contributing significantly to better healthcare outcomes.
1.1. Key Aspects of Software Program Design
- User-Centered Design: Focuses on the needs and workflows of healthcare professionals and patients to ensure usability and efficiency.
- Data Security and Privacy: Employs robust security measures to protect sensitive patient data, complying with regulations such as HIPAA.
- Interoperability: Ensures seamless integration with existing healthcare systems and devices for efficient data exchange.
- Scalability: Designs systems that can handle increasing amounts of data and users as the healthcare organization grows.
- Reliability: Guarantees consistent performance and uptime, minimizing disruptions in critical healthcare operations.
 User-Centered Design for Healthcare Software
User-Centered Design for Healthcare Software
1.2. Types of Healthcare Software
| Software Type | Description |
|---|---|
| Electronic Health Records | Digital versions of patient medical history, crucial for efficient data management and informed decision-making. |
| Telemedicine Platforms | Enables remote consultations and monitoring, extending healthcare access to underserved areas and improving patient convenience. |
| Medical Imaging Software | Aids in processing and analyzing medical images for accurate diagnoses and treatment planning. |
| Medical Billing Software | Automates billing and claims processes, reducing errors and improving revenue cycle management. |
| Remote Patient Monitoring (RPM) | Collects patient data outside traditional healthcare settings, allowing for timely interventions and improved chronic disease management. |
2. Why is Effective Software Program Design Important in Healthcare?
Effective software program design is crucial in healthcare because it enhances patient care, streamlines workflows, ensures data security, and promotes innovation. Well-designed software solutions in healthcare ensure that medical professionals have access to accurate and timely information, which leads to better diagnoses and treatment plans. According to a study published in the Journal of the American Medical Informatics Association, effective EHR systems, for example, reduce medication errors by up to 30% and improve adherence to clinical guidelines by 25%. By optimizing workflows, these systems also free up healthcare providers to focus more on patient interaction and less on administrative tasks.
2.1. Enhancing Patient Care
- Improved Accuracy: Reduces errors in diagnosis and treatment through access to comprehensive patient data.
- Better Coordination: Facilitates seamless communication and collaboration among healthcare providers.
- Personalized Treatment: Enables tailored treatment plans based on individual patient needs and preferences.
2.2. Streamlining Workflows
- Automation: Automates repetitive tasks, such as appointment scheduling and billing, saving time and resources.
- Efficiency: Optimizes processes, reducing bottlenecks and improving overall productivity.
- Resource Management: Enhances the allocation and utilization of resources, such as staff and equipment.
2.3. Ensuring Data Security
- Compliance: Adheres to regulatory requirements, such as HIPAA, to protect patient privacy and data security.
- Protection: Employs advanced security measures to safeguard against unauthorized access and cyber threats.
- Integrity: Maintains the accuracy and reliability of patient data.
2.4. Promoting Innovation
- Research: Facilitates medical research and development through data analysis and knowledge sharing.
- New Technologies: Drives the adoption of innovative technologies, such as AI and machine learning, in healthcare.
- Continuous Improvement: Supports ongoing efforts to improve healthcare delivery and patient outcomes.
3. How Does Software Program Design Improve Patient Outcomes?
Software program design directly enhances patient outcomes by improving diagnostic accuracy, treatment effectiveness, patient engagement, and access to care. Well-designed healthcare software ensures that medical professionals can make informed decisions based on comprehensive patient data, leading to more accurate diagnoses and better treatment plans. A 2023 report by the Agency for Healthcare Research and Quality (AHRQ) indicates that the use of clinical decision support systems (CDSS) within EHRs can improve the quality of care by providing evidence-based recommendations and alerts to healthcare providers.
3.1. Diagnostic Accuracy
- Data Integration: Consolidates patient information from various sources to provide a complete medical history.
- Decision Support: Offers real-time clinical decision support to guide diagnostic processes.
- Error Reduction: Minimizes diagnostic errors through automated checks and alerts.
3.2. Treatment Effectiveness
- Personalized Plans: Develops tailored treatment plans based on individual patient needs and preferences.
- Medication Management: Optimizes medication management to reduce adverse drug events and improve adherence.
- Outcome Monitoring: Tracks treatment outcomes and adjusts plans as necessary.
3.3. Patient Engagement
- Access to Information: Empowers patients with access to their medical records and educational resources.
- Communication Tools: Provides secure communication channels for patients to interact with their healthcare providers.
- Remote Monitoring: Facilitates remote monitoring of patient health metrics for timely interventions.
3.4. Access to Care
- Telemedicine: Expands access to care for patients in remote or underserved areas through virtual consultations.
- Appointment Management: Streamlines appointment scheduling and reduces wait times.
- Care Coordination: Improves care coordination among different healthcare providers and settings.
4. What are the Key Components of Healthcare Software Program Design?
The key components of healthcare software program design include user interface (UI) design, data management, security protocols, interoperability standards, and compliance regulations. Each of these components is critical to ensuring that the software is effective, secure, and compliant with healthcare industry standards. A well-designed user interface ensures that healthcare professionals can easily navigate and use the software, while robust data management systems ensure the accuracy and reliability of patient information.
4.1. User Interface (UI) Design
- Intuitive Navigation: Provides easy-to-understand navigation and layout.
- Accessibility: Ensures the software is accessible to users with disabilities, compliant with WCAG guidelines.
- Customization: Allows users to customize the interface to suit their preferences and workflows.
4.2. Data Management
- Data Storage: Utilizes secure and scalable data storage solutions to manage large volumes of patient data.
- Data Integrity: Implements data validation and quality control measures to ensure data accuracy.
- Data Retrieval: Provides efficient data retrieval mechanisms for quick access to patient information.
4.3. Security Protocols
- Access Control: Restricts access to sensitive data based on user roles and permissions.
- Encryption: Encrypts data both in transit and at rest to protect against unauthorized access.
- Audit Trails: Maintains detailed audit trails to track user activity and detect potential security breaches.
4.4. Interoperability Standards
- HL7 Compliance: Adheres to HL7 standards for exchanging healthcare information between different systems.
- FHIR Support: Supports FHIR (Fast Healthcare Interoperability Resources) for modern and flexible data exchange.
- API Integration: Provides APIs for seamless integration with other healthcare applications and devices.
4.5. Compliance Regulations
- HIPAA Compliance: Ensures compliance with HIPAA regulations to protect patient privacy and data security.
- GDPR Compliance: Adheres to GDPR guidelines for handling personal data of EU citizens.
- FDA Regulations: Complies with FDA regulations for medical devices and software.
5. How Do You Ensure Data Security in Healthcare Software Design?
Ensuring data security in healthcare software design involves implementing robust security protocols, adhering to compliance regulations, conducting regular security audits, and providing ongoing security training. Protecting patient data is paramount in healthcare, and software design must incorporate multiple layers of security to prevent breaches and maintain patient trust. According to a 2024 report by the U.S. Department of Health and Human Services (HHS), data breaches in healthcare can lead to significant financial losses, reputational damage, and compromised patient care.
5.1. Robust Security Protocols
- Access Control: Implementing role-based access control to limit data access to authorized personnel only.
- Encryption: Using strong encryption algorithms to protect data both in transit and at rest.
- Firewalls: Deploying firewalls to prevent unauthorized access to the network.
- Intrusion Detection Systems: Monitoring network traffic for suspicious activity and potential security breaches.
5.2. Compliance Regulations
- HIPAA Compliance: Adhering to the Health Insurance Portability and Accountability Act (HIPAA) regulations to protect patient privacy and data security.
- GDPR Compliance: Complying with the General Data Protection Regulation (GDPR) for handling personal data of EU citizens.
- NIST Guidelines: Following the National Institute of Standards and Technology (NIST) guidelines for cybersecurity best practices.
5.3. Regular Security Audits
- Vulnerability Assessments: Conducting regular vulnerability assessments to identify potential security weaknesses.
- Penetration Testing: Performing penetration testing to simulate cyber attacks and evaluate the effectiveness of security measures.
- Security Code Reviews: Conducting thorough security code reviews to identify and fix vulnerabilities in the software.
5.4. Ongoing Security Training
- Employee Training: Providing regular security training to employees to raise awareness about potential threats and best practices for data protection.
- Phishing Simulations: Conducting phishing simulations to test employees’ ability to recognize and avoid phishing attacks.
- Incident Response Planning: Developing and regularly updating incident response plans to effectively handle security breaches.
6. What Role Does Interoperability Play in Healthcare Software Program Design?
Interoperability is essential in healthcare software program design because it enables seamless data exchange between different systems, improves care coordination, and enhances overall efficiency. Interoperability ensures that patient information can be easily shared among various healthcare providers and systems, leading to better-informed decisions and improved patient outcomes. According to a 2022 report by the Office of the National Coordinator for Health Information Technology (ONC), interoperable systems reduce administrative costs, improve patient safety, and enhance the quality of care.
6.1. Seamless Data Exchange
- HL7 Standards: Using HL7 (Health Level Seven) standards to enable the exchange of structured healthcare information.
- FHIR Support: Supporting FHIR (Fast Healthcare Interoperability Resources) for modern and flexible data exchange.
- API Integration: Providing APIs (Application Programming Interfaces) for seamless integration with other healthcare applications and devices.
6.2. Improved Care Coordination
- Data Sharing: Facilitating the sharing of patient data among different healthcare providers and settings.
- Care Plans: Enabling the creation and sharing of coordinated care plans.
- Referral Management: Streamlining the referral management process to ensure continuity of care.
6.3. Enhanced Efficiency
- Automation: Automating data exchange processes to reduce manual effort and errors.
- Real-Time Access: Providing real-time access to patient information for timely decision-making.
- Reduced Redundancy: Eliminating redundant data entry and improving data accuracy.
7. How Can AI and Machine Learning Enhance Healthcare Software Program Design?
AI and machine learning (ML) significantly enhance healthcare software program design by improving diagnostic accuracy, personalizing treatment plans, automating administrative tasks, and enhancing research capabilities. These technologies enable software to analyze vast amounts of data, identify patterns, and provide insights that can improve patient care and operational efficiency. According to a 2023 report by McKinsey, AI and ML have the potential to save the healthcare industry billions of dollars annually while significantly improving patient outcomes.
7.1. Diagnostic Accuracy
- Image Analysis: Using AI to analyze medical images, such as X-rays and MRIs, to detect diseases and abnormalities.
- Predictive Analytics: Applying machine learning algorithms to predict the likelihood of disease based on patient data.
- Clinical Decision Support: Providing AI-powered clinical decision support to guide diagnostic processes.
7.2. Personalized Treatment Plans
- Data Analysis: Analyzing patient data to identify individual treatment needs and preferences.
- Treatment Optimization: Optimizing treatment plans based on predicted outcomes.
- Medication Management: Personalizing medication dosages and schedules to improve adherence and reduce adverse effects.
7.3. Automation of Administrative Tasks
- Appointment Scheduling: Automating appointment scheduling and reminders.
- Billing and Claims Processing: Streamlining billing and claims processing.
- Data Entry: Automating data entry to reduce manual effort and errors.
7.4. Enhanced Research Capabilities
- Data Mining: Mining large datasets to identify patterns and trends in disease occurrence and treatment outcomes.
- Drug Discovery: Accelerating the drug discovery process through AI-powered analysis of molecular structures and biological pathways.
- Clinical Trial Optimization: Optimizing clinical trial design and patient recruitment.
8. What are the Challenges in Healthcare Software Program Design?
Challenges in healthcare software program design include ensuring data security and privacy, achieving interoperability, managing regulatory compliance, and addressing usability issues. These challenges require careful planning, robust security measures, and a deep understanding of the healthcare industry’s unique requirements. According to a 2024 report by Deloitte, overcoming these challenges is critical for realizing the full potential of healthcare software and improving patient outcomes.
8.1. Data Security and Privacy
- Data Breaches: Protecting against data breaches and unauthorized access to sensitive patient information.
- Compliance: Complying with HIPAA and other regulatory requirements for data protection.
- Data Encryption: Implementing strong encryption to protect data both in transit and at rest.
8.2. Interoperability
- Data Exchange: Achieving seamless data exchange between different healthcare systems and providers.
- Standardization: Adhering to interoperability standards, such as HL7 and FHIR.
- Integration: Integrating with legacy systems and new technologies.
8.3. Regulatory Compliance
- HIPAA Compliance: Ensuring compliance with HIPAA regulations for patient privacy and data security.
- FDA Regulations: Complying with FDA regulations for medical devices and software.
- GDPR Compliance: Adhering to GDPR guidelines for handling personal data of EU citizens.
8.4. Usability Issues
- User-Friendly Design: Creating software that is easy to use and navigate for healthcare professionals.
- Accessibility: Ensuring the software is accessible to users with disabilities.
- Workflow Integration: Integrating the software seamlessly into existing clinical workflows.
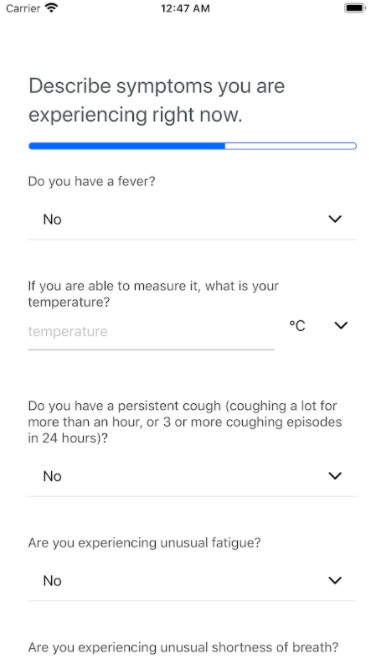
9. How Do Mobile Health (mHealth) Apps Fit Into Healthcare Software Program Design?
Mobile health (mHealth) apps are an integral part of healthcare software program design, offering solutions for remote patient monitoring, medication management, telehealth services, and health and wellness tracking. These apps empower patients to take control of their health, improve adherence to treatment plans, and communicate more effectively with their healthcare providers. According to a 2023 report by Statista, the mHealth market is projected to reach $189 billion by 2025, driven by increasing adoption of smartphones and growing demand for remote healthcare services.
9.1. Remote Patient Monitoring
- Wearable Devices: Integrating with wearable devices to track vital signs and activity levels.
- Data Collection: Collecting and transmitting patient data to healthcare providers in real-time.
- Alert Systems: Providing alerts to healthcare providers when patient data indicates a potential problem.
9.2. Medication Management
- Reminder Systems: Providing reminders to patients to take their medications.
- Adherence Tracking: Tracking patient adherence to medication schedules.
- Drug Information: Providing information about medications, including dosages, side effects, and interactions.
9.3. Telehealth Services
- Virtual Consultations: Enabling virtual consultations with healthcare providers.
- Remote Diagnostics: Providing tools for remote diagnostics and monitoring.
- Secure Communication: Offering secure communication channels for patients to interact with their healthcare providers.
9.4. Health and Wellness Tracking
- Fitness Tracking: Tracking physical activity, sleep patterns, and nutrition.
- Goal Setting: Helping patients set and track health and wellness goals.
- Educational Resources: Providing educational resources and support for healthy lifestyle choices.
 Mobile Health App
Mobile Health App
10. What Future Trends Will Shape Healthcare Software Program Design?
Future trends shaping healthcare software program design include increased use of AI and machine learning, adoption of blockchain technology, expansion of telehealth services, and a greater focus on personalized medicine. These trends promise to transform healthcare delivery, improve patient outcomes, and enhance the efficiency of healthcare systems. According to a 2024 report by Accenture, these trends will drive significant innovation and investment in the healthcare software market over the next decade.
10.1. Increased Use of AI and Machine Learning
- Advanced Diagnostics: AI-powered tools for more accurate and efficient diagnostics.
- Personalized Treatment: Machine learning algorithms for personalized treatment plans.
- Predictive Analytics: Predictive models for identifying patients at risk of developing diseases.
10.2. Adoption of Blockchain Technology
- Secure Data Sharing: Blockchain for secure and transparent data sharing among healthcare providers.
- Supply Chain Management: Blockchain for tracking and managing the supply chain of pharmaceuticals and medical devices.
- Identity Management: Blockchain for secure identity management of patients and healthcare providers.
10.3. Expansion of Telehealth Services
- Remote Monitoring: Remote patient monitoring through wearable devices and mobile apps.
- Virtual Consultations: Virtual consultations with healthcare providers for routine check-ups and specialized care.
- Telepharmacy: Telepharmacy services for remote medication dispensing and counseling.
10.4. Greater Focus on Personalized Medicine
- Genomic Data: Integration of genomic data into treatment plans.
- Precision Medicine: Personalized treatment approaches based on individual patient characteristics.
- Data Analytics: Advanced data analytics for identifying the most effective treatments for specific patient populations.
CAR-REMOTE-REPAIR.EDU.VN is committed to staying at the forefront of these trends, providing cutting-edge training and support to healthcare professionals. To explore how our programs can enhance your skills in healthcare software program design, visit our website or contact us directly. Address: 1700 W Irving Park Rd, Chicago, IL 60613, United States. Whatsapp: +1 (641) 206-8880. Website: CAR-REMOTE-REPAIR.EDU.VN.
FAQ: Software Program Design on Health Care
1. What is the primary goal of software program design in healthcare?
The primary goal is to improve patient care and operational efficiency by creating effective and secure software solutions tailored to the healthcare industry.
2. How does effective software program design contribute to better patient outcomes?
It ensures accurate diagnoses, personalized treatment plans, improved patient engagement, and enhanced access to care.
3. What are the key components of healthcare software program design?
Key components include user interface (UI) design, data management, security protocols, interoperability standards, and compliance regulations.
4. How do you ensure data security in healthcare software design?
By implementing robust security protocols, adhering to compliance regulations, conducting regular security audits, and providing ongoing security training.
5. Why is interoperability important in healthcare software program design?
It enables seamless data exchange between different systems, improves care coordination, and enhances overall efficiency.
6. What role do AI and machine learning play in healthcare software program design?
They improve diagnostic accuracy, personalize treatment plans, automate administrative tasks, and enhance research capabilities.
7. What are the main challenges in healthcare software program design?
Challenges include ensuring data security and privacy, achieving interoperability, managing regulatory compliance, and addressing usability issues.
8. How do mobile health (mHealth) apps fit into healthcare software program design?
They offer solutions for remote patient monitoring, medication management, telehealth services, and health and wellness tracking.
9. What are some future trends that will shape healthcare software program design?
Future trends include increased use of AI and machine learning, adoption of blockchain technology, expansion of telehealth services, and a greater focus on personalized medicine.
10. How can CAR-REMOTE-REPAIR.EDU.VN help me enhance my skills in healthcare software program design?
CAR-REMOTE-REPAIR.EDU.VN offers cutting-edge training and support to healthcare professionals, helping them stay at the forefront of healthcare technology. Visit our website or contact us directly to explore our programs.