Care Management Software Healthcare revolutionizes patient care by centralizing data, streamlining workflows, and improving communication, and CAR-REMOTE-REPAIR.EDU.VN offers training to master this vital technology. By implementing this software, healthcare providers can deliver more coordinated, efficient, and personalized care, leading to better patient outcomes and satisfaction. This article explores the definition, application, and benefits of care management software in healthcare, including care coordination platforms and electronic health record (EHR) integration.
Contents
- 1. What Is Care Management Software in Healthcare?
- 1.1. Why Is Care Management Software Important in Healthcare?
- 1.2. What Are the Key Components of Care Management Software?
- 2. What Are the Primary Features of Care Management Software in Healthcare?
- 2.1. Patient Tracking and Monitoring
- 2.2. Care Planning and Coordination
- 2.3. Communication and Collaboration Tools
- 2.4. Reporting and Analytics
- 3. What Are the Benefits of Using Care Management Software in Healthcare?
- 3.1. Improved Care Coordination
- 3.2. Enhanced Patient Engagement
- 3.3. Reduced Healthcare Costs
- 3.4. Better Patient Outcomes
- 4. How to Implement Care Management Software in Healthcare?
- 4.1. Assess Your Needs and Goals
- 4.2. Select the Right Software
- 4.3. Integrate with Existing Systems
- 4.4. Train Staff
- 4.5. Monitor Performance
- 5. What Are the Challenges of Implementing Care Management Software in Healthcare?
- 5.1. Data Integration Issues
- 5.2. Resistance to Change
- 5.3. Need for Ongoing Training and Support
- 6. What Are the Current Trends in Care Management Software Healthcare?
- 6.1. Increased Use of AI and Machine Learning
1. What Is Care Management Software in Healthcare?
Care management software healthcare is a technological solution designed to streamline and enhance the delivery of patient care. It centralizes patient information, automates administrative tasks, and facilitates communication among healthcare providers, ultimately improving patient outcomes.
Care management software healthcare involves using specialized tools to coordinate and oversee a patient’s medical care. According to a study by the National Institutes of Health, these platforms are designed to enhance the quality and efficiency of healthcare services by improving communication and coordination among healthcare providers. Care management software systems provide a centralized platform for managing patient data, scheduling appointments, tracking medications, and monitoring patient progress. This technology enables healthcare professionals to deliver more coordinated, efficient, and personalized care, leading to better patient outcomes and increased patient satisfaction. As healthcare continues to evolve, care management software remains an essential tool for modern healthcare providers aiming to optimize their services.
1.1. Why Is Care Management Software Important in Healthcare?
Care management software is important in healthcare because it improves care coordination, reduces healthcare costs, and enhances patient outcomes. According to research from the Agency for Healthcare Research and Quality (AHRQ), effective care management programs can significantly improve chronic disease management and reduce hospital readmissions.
The implementation of care management software healthcare provides numerous benefits:
- Improved Care Coordination: Care management software facilitates seamless communication and collaboration among healthcare providers, ensuring that all members of the care team are informed and aligned regarding the patient’s treatment plan. This can be especially helpful for patients with chronic conditions who may see multiple specialists.
- Reduced Healthcare Costs: By proactively managing patient care and preventing unnecessary hospital visits, care management software helps reduce healthcare costs. For example, it can identify patients at high risk for hospital readmission and implement interventions to prevent such occurrences.
- Enhanced Patient Outcomes: Care management software enables healthcare providers to deliver more personalized and proactive care, leading to improved patient outcomes. Features like remote monitoring and medication management help patients stay on track with their treatment plans and improve their overall health.
- Streamlined Workflows: By automating administrative tasks and providing a centralized platform for managing patient data, care management software streamlines workflows for healthcare providers. This allows them to focus more on direct patient care, improving efficiency and job satisfaction.
- Data-Driven Insights: Care management software provides valuable data and analytics that can be used to improve care delivery. By tracking key performance indicators and identifying trends, healthcare providers can make data-driven decisions to optimize their care management programs.
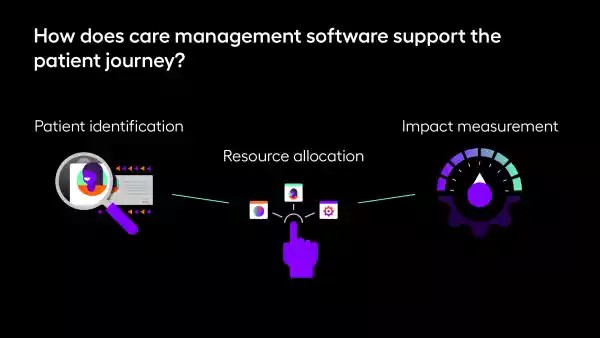 Diagram illustrating the support of the patient journey using care management software with patient identification, resource allocation, and impact measurement
Diagram illustrating the support of the patient journey using care management software with patient identification, resource allocation, and impact measurement
1.2. What Are the Key Components of Care Management Software?
The key components of care management software typically include patient portals, care plans, task management tools, and reporting features. According to a report by HIMSS, these components are essential for effective care coordination and patient engagement.
Care management software comprises several essential features that work together to improve patient care. Here are some key components:
- Patient Portal: A secure online portal that allows patients to access their medical records, schedule appointments, communicate with healthcare providers, and request medication refills. This empowers patients to take an active role in their healthcare.
- Care Plans: Customizable care plans that outline the patient’s treatment goals, interventions, and progress. These plans can be tailored to meet the individual needs of each patient and are easily accessible to all members of the care team.
- Task Management Tools: Features that allow care managers to assign tasks, track progress, and set reminders for important activities such as follow-up appointments, medication refills, and lab tests.
- Reporting and Analytics: Tools that provide insights into patient outcomes, program performance, and cost savings. These reports can be used to identify areas for improvement and track the effectiveness of care management interventions.
- Integration Capabilities: The ability to integrate with other healthcare systems, such as electronic health records (EHRs), billing systems, and pharmacy databases. This ensures seamless data exchange and eliminates the need for manual data entry.
- Communication Tools: Secure messaging and video conferencing capabilities that allow care team members to communicate with each other and with patients. This promotes collaboration and ensures that everyone is on the same page.
- Remote Monitoring: Integration with remote monitoring devices, such as wearable sensors and home health monitors, to track patient vital signs and other health metrics. This allows for early detection of potential health problems and proactive intervention.
- Medication Management: Features that help patients manage their medications, including medication reminders, refill requests, and drug interaction alerts. This reduces the risk of medication errors and improves adherence to treatment plans.
2. What Are the Primary Features of Care Management Software in Healthcare?
The primary features of care management software in healthcare include patient tracking, care planning, communication tools, and reporting capabilities. These features help healthcare providers deliver comprehensive and coordinated care.
Effective care management software offers a range of features designed to streamline and enhance the delivery of healthcare services. These features typically include tools for patient tracking, care planning, communication, and reporting. Let’s take a closer look at each of these key components:
2.1. Patient Tracking and Monitoring
Patient tracking and monitoring features allow healthcare providers to monitor patient progress, track key health metrics, and identify potential issues early on. According to a study published in the Journal of the American Medical Informatics Association, remote patient monitoring can significantly improve outcomes for patients with chronic conditions.
Care management software healthcare offers robust patient tracking and monitoring capabilities that enable healthcare providers to stay informed about their patients’ health status and progress. These features typically include:
- Real-Time Data Monitoring: Integration with remote monitoring devices, such as wearable sensors and home health monitors, allows for continuous monitoring of patient vital signs and other health metrics.
- Alerts and Notifications: Automated alerts and notifications that are triggered when patient data falls outside of pre-defined parameters. This enables healthcare providers to intervene promptly and prevent potential health crises.
- Patient History Tracking: Comprehensive tracking of patient medical history, including diagnoses, medications, allergies, and previous treatments. This provides a complete picture of the patient’s health status and helps inform care decisions.
- Appointment Scheduling: Integrated appointment scheduling features that allow healthcare providers to schedule and manage patient appointments efficiently. This ensures that patients receive timely care and reduces the risk of missed appointments.
- Medication Management: Tools that help patients manage their medications, including medication reminders, refill requests, and drug interaction alerts. This reduces the risk of medication errors and improves adherence to treatment plans.
- Progress Tracking: Features that allow healthcare providers to track patient progress towards their treatment goals and identify any barriers to success. This enables them to adjust care plans as needed and ensure that patients are on track to achieve their desired outcomes.
2.2. Care Planning and Coordination
Care planning and coordination features enable healthcare providers to develop and implement individualized care plans, coordinate services, and ensure continuity of care. Research from the Centers for Medicare & Medicaid Services (CMS) shows that comprehensive care planning can improve patient outcomes and reduce healthcare costs.
Care management software healthcare includes features for care planning and coordination, which allow healthcare providers to develop and implement individualized care plans for their patients. These features typically include:
- Care Plan Templates: Customizable care plan templates that can be tailored to meet the specific needs of each patient. These templates provide a framework for developing comprehensive care plans that address the patient’s medical, social, and behavioral health needs.
- Goal Setting: Features that allow healthcare providers to collaborate with patients to set realistic and achievable goals for their treatment. This empowers patients to take an active role in their care and increases their motivation to adhere to their treatment plans.
- Task Assignment: Tools that allow care managers to assign tasks to members of the care team and track progress towards completion. This ensures that all members of the care team are working together effectively to meet the patient’s needs.
- Care Coordination: Features that facilitate communication and collaboration among healthcare providers, ensuring that all members of the care team are informed and aligned regarding the patient’s treatment plan. This is particularly important for patients with complex medical needs who may see multiple specialists.
- Resource Management: Tools that help healthcare providers identify and connect patients with community resources, such as transportation assistance, food banks, and support groups. This helps address social determinants of health and improve patient outcomes.
- Progress Monitoring: Features that allow healthcare providers to monitor patient progress towards their treatment goals and identify any barriers to success. This enables them to adjust care plans as needed and ensure that patients are on track to achieve their desired outcomes.
2.3. Communication and Collaboration Tools
Communication and collaboration tools facilitate secure communication among healthcare providers, patients, and caregivers, ensuring everyone is informed and involved in the care process. According to a study in Health Affairs, effective communication can improve patient safety and reduce medical errors.
Care management software healthcare offers a range of communication and collaboration tools that facilitate secure and efficient communication among healthcare providers, patients, and caregivers. These tools typically include:
- Secure Messaging: HIPAA-compliant messaging that allows healthcare providers to communicate with each other and with patients in a secure and confidential manner. This eliminates the need for email or phone calls and ensures that patient information is protected.
- Video Conferencing: Video conferencing capabilities that allow healthcare providers to conduct virtual consultations with patients, assess their condition, and provide education and support. This is particularly useful for patients who live in rural areas or have difficulty traveling to appointments.
- Care Team Collaboration: Features that allow members of the care team to share information, discuss patient cases, and coordinate care activities in real-time. This ensures that everyone is on the same page and that patients receive seamless and coordinated care.
- Patient Portal: A secure online portal that allows patients to access their medical records, schedule appointments, communicate with healthcare providers, and request medication refills. This empowers patients to take an active role in their healthcare and improves their satisfaction with the care they receive.
- Automated Notifications: Automated notifications that remind patients of upcoming appointments, medication refills, and other important activities. This helps improve adherence to treatment plans and reduces the risk of missed appointments.
- Integration with EHRs: Integration with electronic health records (EHRs) that allows healthcare providers to access patient information directly from the care management platform. This eliminates the need for manual data entry and ensures that patient information is accurate and up-to-date.
2.4. Reporting and Analytics
Reporting and analytics features provide insights into patient outcomes, program performance, and cost savings, enabling healthcare providers to make data-driven decisions and improve care delivery. Research from the National Committee for Quality Assurance (NCQA) highlights the importance of data analytics in improving healthcare quality.
Care management software healthcare includes robust reporting and analytics features that provide insights into patient outcomes, program performance, and cost savings. These features enable healthcare providers to make data-driven decisions and continuously improve the quality of care they provide. Here are some common reporting and analytics capabilities:
- Outcome Tracking: Monitoring key performance indicators (KPIs) such as hospital readmission rates, emergency department visits, and patient satisfaction scores. This allows healthcare providers to assess the effectiveness of their care management programs and identify areas for improvement.
- Program Performance: Analyzing program participation rates, engagement levels, and adherence to treatment plans. This helps healthcare providers understand how well their programs are reaching and engaging patients and identify strategies for improving participation and adherence.
- Cost Analysis: Evaluating the cost-effectiveness of care management programs by tracking expenses, savings, and return on investment (ROI). This helps healthcare providers justify the value of their programs and demonstrate their impact on the bottom line.
- Risk Stratification: Identifying high-risk patients who are most likely to benefit from care management interventions. This allows healthcare providers to prioritize their resources and focus on patients who need the most support.
- Trend Analysis: Identifying trends and patterns in patient data to predict future health outcomes and proactively address potential issues. This enables healthcare providers to deliver more personalized and preventive care.
- Customizable Reports: Creating custom reports that meet the specific needs of the healthcare organization. This allows healthcare providers to track the metrics that are most important to them and gain insights into the areas they are most interested in.
3. What Are the Benefits of Using Care Management Software in Healthcare?
The benefits of using care management software in healthcare include improved care coordination, enhanced patient engagement, reduced healthcare costs, and better patient outcomes. These advantages make care management software a valuable tool for healthcare providers.
Care management software healthcare offers a multitude of benefits that can transform the way healthcare is delivered. From improved care coordination to reduced costs, the advantages of implementing such a system are significant. Let’s delve into the key benefits:
3.1. Improved Care Coordination
Care management software improves care coordination by facilitating seamless communication and collaboration among healthcare providers, patients, and caregivers. According to a study in Medical Care, better care coordination leads to fewer medical errors and improved patient satisfaction.
Care management software plays a vital role in improving care coordination by providing a centralized platform for managing patient information and facilitating communication among healthcare providers, patients, and caregivers. Some specific ways in which care management software enhances care coordination include:
- Centralized Patient Information: Care management software provides a single, comprehensive view of the patient’s medical history, including diagnoses, medications, allergies, and previous treatments. This ensures that all members of the care team have access to the most up-to-date information, regardless of where the patient receives care.
- Streamlined Communication: Care management software facilitates secure and efficient communication among healthcare providers, patients, and caregivers. This allows for timely exchange of information and ensures that everyone is on the same page regarding the patient’s treatment plan.
- Care Plan Coordination: Care management software enables healthcare providers to develop and implement individualized care plans that are tailored to meet the specific needs of each patient. These care plans can be shared with all members of the care team, ensuring that everyone is working together towards the same goals.
- Task Management: Care management software includes task management features that allow care managers to assign tasks to members of the care team and track progress towards completion. This ensures that all necessary tasks are completed in a timely manner and that patients receive the care they need.
- Appointment Scheduling: Care management software provides integrated appointment scheduling features that allow healthcare providers to schedule and manage patient appointments efficiently. This ensures that patients receive timely care and reduces the risk of missed appointments.
- Referral Management: Care management software facilitates the referral process by allowing healthcare providers to easily refer patients to specialists and other healthcare services. This ensures that patients receive the appropriate care in a timely manner.
3.2. Enhanced Patient Engagement
Care management software enhances patient engagement by empowering patients to take an active role in their care through patient portals, educational resources, and communication tools. Research from the Patient Engagement Framework shows that engaged patients have better health outcomes and are more satisfied with their care.
Care management software plays a crucial role in enhancing patient engagement by providing tools and resources that empower patients to take an active role in their healthcare. Some specific ways in which care management software promotes patient engagement include:
- Patient Portals: Secure online portals that allow patients to access their medical records, schedule appointments, communicate with healthcare providers, and request medication refills. This gives patients greater control over their healthcare and empowers them to make informed decisions about their treatment.
- Educational Resources: Access to a library of educational materials, including articles, videos, and interactive tools, that help patients learn about their health conditions and how to manage them effectively. This empowers patients to take better care of themselves and make informed decisions about their healthcare.
- Communication Tools: Secure messaging and video conferencing capabilities that allow patients to communicate with their healthcare providers and receive remote support and education. This improves patient access to care and enhances their satisfaction with the care they receive.
- Personalized Care Plans: Care plans that are tailored to meet the individual needs of each patient and are developed in collaboration with the patient and their healthcare providers. This ensures that patients are actively involved in their care and that their preferences and values are taken into account.
- Remote Monitoring: Integration with remote monitoring devices, such as wearable sensors and home health monitors, that allow patients to track their health metrics and share them with their healthcare providers. This empowers patients to take an active role in managing their health and provides valuable data to their healthcare providers.
- Feedback and Surveys: Opportunities for patients to provide feedback on their care and share their experiences with their healthcare providers. This helps healthcare providers improve the quality of their services and ensure that they are meeting the needs of their patients.
3.3. Reduced Healthcare Costs
Care management software reduces healthcare costs by preventing unnecessary hospital visits, improving medication adherence, and optimizing resource utilization. A study by the Brookings Institution found that effective care management programs can significantly reduce healthcare spending.
Care management software plays a key role in reducing healthcare costs by preventing unnecessary hospital visits, improving medication adherence, and optimizing resource utilization. Here are some specific ways in which care management software helps to lower healthcare expenses:
- Preventing Hospital Readmissions: By proactively monitoring patients’ health and providing timely interventions, care management software can help prevent hospital readmissions. This not only improves patient outcomes but also reduces the cost of unnecessary hospital stays.
- Improving Medication Adherence: Care management software includes features such as medication reminders and refill requests that help patients stay on track with their medications. This reduces the risk of medication-related complications and hospitalizations, leading to lower healthcare costs.
- Optimizing Resource Utilization: Care management software helps healthcare providers allocate their resources more efficiently by identifying patients who are most likely to benefit from care management interventions. This ensures that resources are targeted to the patients who need them most, reducing waste and improving the overall efficiency of the healthcare system.
- Reducing Emergency Department Visits: By providing patients with access to timely and appropriate care, care management software can help reduce the number of unnecessary emergency department visits. This not only lowers healthcare costs but also frees up valuable resources for patients who truly need emergency care.
- Streamlining Administrative Processes: Care management software automates many administrative tasks, such as appointment scheduling and billing, which reduces administrative costs and frees up staff time for other important activities.
- Promoting Preventive Care: By providing patients with access to educational resources and personalized care plans, care management software encourages them to engage in preventive care activities, such as screenings and vaccinations. This can help prevent the onset of chronic diseases and reduce the need for costly medical interventions in the future.
3.4. Better Patient Outcomes
Care management software leads to better patient outcomes by providing comprehensive, coordinated, and personalized care that addresses patients’ individual needs. According to a meta-analysis in the Journal of General Internal Medicine, care management programs are associated with significant improvements in health outcomes for patients with chronic conditions.
Care management software is instrumental in achieving better patient outcomes by enabling comprehensive, coordinated, and personalized care tailored to each patient’s specific needs. Here are several ways in which care management software contributes to improved patient health:
- Personalized Care Plans: Care management software enables healthcare providers to create personalized care plans that take into account each patient’s unique medical history, lifestyle, and preferences. This ensures that patients receive the most appropriate and effective care for their individual needs.
- Timely Interventions: By proactively monitoring patients’ health and identifying potential issues early on, care management software allows healthcare providers to intervene in a timely manner. This can prevent minor health problems from escalating into more serious and costly conditions.
- Improved Communication: Care management software facilitates seamless communication among healthcare providers, patients, and caregivers. This ensures that everyone is on the same page and that patients receive consistent and coordinated care.
- Enhanced Self-Management: Care management software provides patients with the tools and resources they need to manage their own health effectively. This includes access to educational materials, medication reminders, and remote monitoring devices.
- Continuity of Care: Care management software helps ensure continuity of care by tracking patient progress and coordinating services across different healthcare settings. This reduces the risk of gaps in care and ensures that patients receive the support they need to stay healthy.
- Data-Driven Insights: Care management software provides healthcare providers with valuable data and analytics that can be used to improve care delivery. This includes tracking key performance indicators, identifying trends, and measuring the impact of care management interventions.
4. How to Implement Care Management Software in Healthcare?
Implementing care management software in healthcare involves assessing needs, selecting the right software, integrating with existing systems, training staff, and monitoring performance. Careful planning and execution are essential for a successful implementation.
Implementing care management software healthcare requires a strategic and well-coordinated approach. The process involves several key steps, from assessing your organization’s needs to training staff and monitoring performance. Let’s break down the essential steps for a successful implementation:
4.1. Assess Your Needs and Goals
Assess your needs and goals by identifying the specific challenges you want to address with care management software and defining clear, measurable objectives for the implementation. According to a guide from the Agency for Healthcare Research and Quality (AHRQ), this assessment is crucial for selecting the right software and ensuring a successful implementation.
Before diving into the implementation of care management software, it is essential to conduct a thorough assessment of your organization’s needs and goals. This involves identifying the specific challenges you want to address with the software and defining clear, measurable objectives for the implementation. Here are some key steps to take during the assessment process:
- Identify Pain Points: Conduct interviews and surveys with healthcare providers, staff, and patients to identify the key pain points in your current care management processes. This could include issues such as poor care coordination, high rates of hospital readmission, or low patient engagement.
- Define Objectives: Based on the identified pain points, define clear, measurable objectives for the implementation of care management software. These objectives should be specific, measurable, achievable, relevant, and time-bound (SMART).
- Assess Current Systems: Evaluate your current healthcare systems and processes to determine how care management software can best integrate with and enhance them. This includes assessing your electronic health record (EHR) system, billing system, and other relevant technologies.
- Consider Stakeholder Needs: Take into account the needs and perspectives of all stakeholders, including healthcare providers, staff, patients, and administrators. This will help ensure that the software is user-friendly and meets the needs of everyone involved.
- Prioritize Requirements: Prioritize your requirements based on their importance and feasibility. This will help you focus on the most critical features and functionalities when selecting a care management software solution.
- Set a Budget: Determine a realistic budget for the implementation of care management software, including the cost of the software, hardware, training, and ongoing maintenance.
4.2. Select the Right Software
Select the right software by evaluating different options based on your needs, budget, and technical requirements. Consider factors such as ease of use, integration capabilities, and vendor support. According to a report by KLAS Research, choosing the right vendor is critical for maximizing the value of your care management software investment.
Selecting the right care management software healthcare is a critical step in ensuring a successful implementation. With numerous options available in the market, it is essential to carefully evaluate different software solutions based on your organization’s needs, budget, and technical requirements. Here are some key factors to consider when selecting the right software:
- Functionality: Evaluate the features and functionalities offered by different software solutions to ensure that they meet your organization’s specific needs. This includes features such as patient tracking, care planning, communication tools, and reporting capabilities.
- Integration Capabilities: Choose a software solution that can seamlessly integrate with your existing healthcare systems, such as your electronic health record (EHR) system, billing system, and pharmacy database. This will ensure that data can be easily exchanged between systems and that healthcare providers have access to the most up-to-date information.
- Ease of Use: Select a software solution that is user-friendly and intuitive to use. This will reduce the learning curve for healthcare providers and staff and ensure that they can quickly and easily adopt the new system.
- Vendor Support: Consider the level of support offered by the software vendor. This includes technical support, training, and ongoing maintenance. Choose a vendor that has a good reputation for providing reliable and responsive support.
- Security: Ensure that the software solution meets all relevant security and privacy regulations, such as HIPAA. This will protect patient data and ensure that your organization is compliant with legal requirements.
- Cost: Evaluate the total cost of ownership of different software solutions, including the cost of the software, hardware, training, and ongoing maintenance. Choose a solution that fits within your budget and provides good value for your investment.
- Scalability: Select a software solution that can scale to meet your organization’s growing needs. This will ensure that the software can continue to support your care management efforts as your organization expands and evolves.
4.3. Integrate with Existing Systems
Integrate with existing systems by ensuring that the care management software can seamlessly exchange data with your EHR, billing system, and other relevant technologies. According to HIMSS, successful integration is essential for optimizing workflows and improving data accuracy.
Integrating care management software with existing healthcare systems is a crucial step in ensuring a seamless and efficient workflow. The ability for the care management software to exchange data with your electronic health record (EHR), billing system, and other relevant technologies is essential for optimizing operations and improving data accuracy. Here are some key considerations for integrating care management software with existing systems:
- HL7 Compatibility: Ensure that the care management software is compatible with the HL7 (Health Level Seven) standard, which is a set of international standards for the transfer of clinical and administrative data between software applications used by various healthcare providers.
- API Integration: Look for a care management software solution that offers robust API (Application Programming Interface) integration capabilities. This will allow you to seamlessly connect the software with your existing systems and exchange data in real-time.
- Data Mapping: Develop a comprehensive data mapping strategy to ensure that data is accurately transferred between systems. This involves identifying the data fields in each system and mapping them to the corresponding fields in the care management software.
- Testing: Conduct thorough testing of the integration to ensure that data is being accurately transferred and that the systems are working together seamlessly. This includes testing all relevant workflows and scenarios.
- Training: Provide training to healthcare providers and staff on how to use the integrated systems. This will help ensure that they are comfortable using the new system and can effectively leverage its capabilities to improve patient care.
- Security: Ensure that the integration meets all relevant security and privacy regulations, such as HIPAA. This will protect patient data and ensure that your organization is compliant with legal requirements.
- Ongoing Maintenance: Plan for ongoing maintenance of the integration to ensure that it continues to function properly and that any issues are resolved in a timely manner. This includes monitoring the integration for errors and providing regular updates to the software.
4.4. Train Staff
Train staff by providing comprehensive training on how to use the care management software, including its features, workflows, and best practices. According to a study in JMIR Human Factors, adequate training is essential for user adoption and effective utilization of care management software.
Training staff is a critical step in ensuring the successful implementation and adoption of care management software healthcare. Providing comprehensive training on how to use the software, including its features, workflows, and best practices, is essential for empowering healthcare providers and staff to effectively leverage the system to improve patient care. Here are some key considerations for training staff on care management software:
- Develop a Training Plan: Create a detailed training plan that outlines the topics to be covered, the training methods to be used, and the schedule for the training sessions. This will help ensure that the training is well-organized and that all relevant topics are covered.
- Customize Training: Tailor the training to meet the specific needs of different user groups. For example, healthcare providers may need more in-depth training on clinical workflows, while administrative staff may need more training on billing and scheduling.
- Provide Hands-On Training: Offer hands-on training sessions that allow staff to practice using the software in a realistic environment. This will help them become more comfortable and confident using the system.
- Use a Variety of Training Methods: Use a variety of training methods, such as lectures, demonstrations, and simulations, to keep staff engaged and to accommodate different learning styles.
- Provide Ongoing Support: Offer ongoing support to staff after the initial training is complete. This could include access to a help desk, online resources, or refresher training sessions.
- Measure Training Effectiveness: Evaluate the effectiveness of the training by measuring user adoption, satisfaction, and performance. This will help you identify areas for improvement and ensure that the training is meeting the needs of the staff.
- Involve Superusers: Identify superusers within your organization who can serve as champions for the care management software and provide support to their colleagues. These superusers can help to promote the adoption of the software and ensure that it is being used effectively.
4.5. Monitor Performance
Monitor performance by tracking key metrics such as patient outcomes, care coordination efficiency, and cost savings. Use this data to identify areas for improvement and optimize your care management programs. According to the National Committee for Quality Assurance (NCQA), continuous monitoring and improvement are essential for achieving optimal results.
Monitoring the performance of care management software healthcare is crucial for ensuring that it is delivering the expected benefits and for identifying areas for improvement. By tracking key metrics such as patient outcomes, care coordination efficiency, and cost savings, healthcare organizations can assess the effectiveness of their care management programs and optimize their operations. Here are some key considerations for monitoring the performance of care management software:
- Define Key Performance Indicators (KPIs): Identify the KPIs that are most relevant to your organization’s goals and objectives. This could include metrics such as hospital readmission rates, emergency department visits, patient satisfaction scores, and cost per patient.
- Establish Benchmarks: Set benchmarks for each KPI to provide a baseline for measuring performance. These benchmarks should be based on industry standards, historical data, or organizational goals.
- Collect Data: Collect data on a regular basis to track performance against the established benchmarks. This data should be accurate, reliable, and timely.
- Analyze Data: Analyze the data to identify trends, patterns, and outliers. This will help you understand what is working well and what needs improvement.
- Identify Areas for Improvement: Based on the data analysis, identify specific areas where you can improve the performance of your care management programs. This could include changes to workflows, training, or technology.
- Implement Changes: Implement the changes that you have identified and monitor their impact on performance. This will help you ensure that the changes are having the desired effect and that your care management programs are continuously improving.
- Communicate Results: Communicate the results of the performance monitoring to all stakeholders, including healthcare providers, staff, and administrators. This will help ensure that everyone is aware of the progress being made and that they are committed to continuous improvement.
5. What Are the Challenges of Implementing Care Management Software in Healthcare?
The challenges of implementing care management software in healthcare include data integration issues, resistance to change, and the need for ongoing training and support. Addressing these challenges proactively is essential for a successful implementation.
Implementing care management software healthcare can present several challenges that healthcare organizations need to address proactively. These challenges can range from technical issues to organizational barriers and require careful planning and execution to overcome. Let’s examine some of the most common challenges:
5.1. Data Integration Issues
Data integration issues can arise when trying to integrate care management software with existing EHRs and other systems, leading to incomplete or inaccurate data. According to a report by the eHealth Initiative, data integration is one of the biggest challenges facing healthcare organizations today.
One of the most significant challenges in implementing care management software is data integration. Healthcare organizations often struggle to integrate the new software with their existing electronic health records (EHRs) and other systems, leading to incomplete or inaccurate data. Here are some specific data integration issues that healthcare organizations may encounter:
- Lack of Interoperability: Many EHR systems are not designed to easily exchange data with other systems, making it difficult to integrate care management software.
- Data Silos: Data may be stored in different systems and formats, making it difficult to consolidate and analyze.
- Data Mapping: Accurately mapping data fields between systems can be a complex and time-consuming process.
- Data Quality: Data may be incomplete, inaccurate, or inconsistent, which can compromise the integrity of the care management software.
- Security and Privacy: Ensuring that data is securely transferred and protected during integration is essential to comply with HIPAA and other regulations.
- Technical Expertise: Integrating care management software with existing systems requires specialized technical expertise that may not be readily available within the organization.
- Vendor Coordination: Coordinating the integration efforts of multiple vendors can be challenging, especially if they have different timelines and priorities.
5.2. Resistance to Change
Resistance to change from healthcare providers and staff can hinder the adoption of care management software, making it difficult to achieve the desired benefits. According to a study in Health Affairs, organizational culture plays a significant role in the successful implementation of new technologies.
Resistance to change is a common challenge in implementing new technologies in healthcare, including care management software. Healthcare providers and staff may be resistant to adopting new systems and processes due to a variety of factors, such as:
- Lack of Understanding: Staff may not fully understand the benefits of the care management software or how it will improve their workflows.
- Fear of Job Loss: Staff may fear that the new software will automate their jobs and lead to job losses.
- Increased Workload: Staff may perceive that the new software will increase their workload or make their jobs more difficult.
- Lack of Training: Staff may not feel adequately trained to use the new software effectively.
- Disruption of Existing Workflows: The new software may disrupt existing workflows and require staff to change the way they do their jobs.
- Technical Difficulties: Staff may experience technical difficulties or frustrations when using the new software.
- Lack of Involvement: Staff may feel that they were not involved in the decision to implement the new software and that their opinions were not taken into account.
5.3. Need for Ongoing Training and Support
The need for ongoing training and support is essential to ensure that healthcare providers and staff can effectively use the care management software and keep up with updates and new features. According to a report by the American Medical Association (AMA), ongoing training and support are critical for maximizing the value of health IT investments.
The need for ongoing training and support is a critical challenge in implementing and maintaining care management software healthcare. Healthcare providers and staff need continuous training to effectively use the software and stay updated with new features and updates. Here are some reasons why ongoing training and support are essential:
- Software Updates: Care management software is constantly evolving, with new features and updates being released regularly. Ongoing training is necessary to ensure that staff is aware of these changes and knows how to use them effectively.
- Staff Turnover: Healthcare organizations often experience staff turnover, which means that new employees need to be trained on the care management software.
- Changing Workflows: As healthcare practices evolve, workflows may need to be adjusted to accommodate the care management software. Ongoing training is necessary to ensure that staff is aware of these changes and knows how to implement them.
- Technical Issues: Technical issues can arise from time to time, and staff needs to know how to troubleshoot these issues or where to go for help.
- Maximizing Value: Ongoing training and support can help healthcare organizations maximize the value of their care management software investment by ensuring that staff is using the software to its full potential.
- Compliance: Ongoing training is necessary to ensure that staff is aware of and compliant with relevant regulations, such as HIPAA.
- Best Practices: Ongoing training can help staff stay up-to-date on best practices for using the care management software to improve patient care.
6. What Are the Current Trends in Care Management Software Healthcare?
Current trends in care management software healthcare include increased use of AI and machine learning, greater emphasis on patient-centered care, and enhanced integration with telehealth services. These trends are shaping the future of care management.
Care management software healthcare is continuously evolving to meet the changing needs of the healthcare industry. Several key trends are currently shaping the landscape of care management software, including:
6.1. Increased Use of AI and Machine Learning
Increased use of AI and machine learning is being seen to analyze patient data, predict health risks, and personalize care plans, improving efficiency and outcomes. According to a report by MarketsandMarkets, the AI in healthcare market is expected to reach $34 billion by 2025.
One of the most significant trends in care management software is the increased use of artificial intelligence (AI) and machine learning. AI and machine learning technologies are being used to analyze patient data, predict health risks, and personalize care plans. Here are some specific ways in which AI and machine learning are being used in care management software:
- Risk Stratification: AI and machine learning algorithms can be used to analyze patient data and identify individuals who are at high risk for developing certain health conditions or experiencing adverse events.
- Predictive Analytics: AI and machine learning can be used to predict patient outcomes, such as hospital readmissions or emergency department visits. This allows healthcare
